Transjugular Intrahepatic Portosystemic Shunt (TIPS) in Radiology: Practice Essentials, History of TIPS, Indications
Most patients can safely undergo TIPS placement with intravenous conscious sedation involving short-acting benzodiazepines and opiates. Some institutions prefer use of general anesthesia during TIPS procedures because of the prolonged nature of the procedure and the degree of discomfort that many patients experience during transvenous punctures. This technique is fairly standard and has been well described in the scientific literature, with some minor variations related to the interventionalist or the center at which the procedure is performed.
Commercially available sets specifically designed for TIPS placement are available in the United States, such as the following:
-
Colapinto transjugular cholangiography liver biopsy set. This includes a 16-gauge Colapinto puncture needle.
-
Rosch-Uchida transjugular liver access set. This includes a 14-gauge needle with a trocar.
-
AngioDynamics transjugular access set.
-
Ring transjugular intrahepatic access set.
At the author’s institution, the right internal jugular vein is accessed, usually with ultrasonographic guidance. The left jugular vein may be used if the right vein is unsuitable for any reason. Techniques involving a femoral venous approach have been described, but these are used much less commonly and are technically more demanding.
[21, 22, 23]
With standard catheter exchange, a 5F catheter with a multipurpose curve is placed into the right hepatic vein. The catheter is wedged in a peripheral branch of the right hepatic vein. Wedged hepatic venography is then performed with carbon dioxide gas to opacify the portal venous system.
(See the images below.)
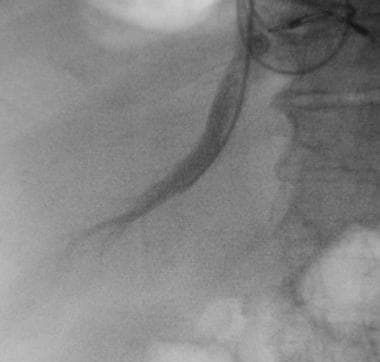
Basic transjugular intrahepatic portosystemic shunt (TIPS) procedure. A curved catheter is placed into the right hepatic vein.
View Media Gallery
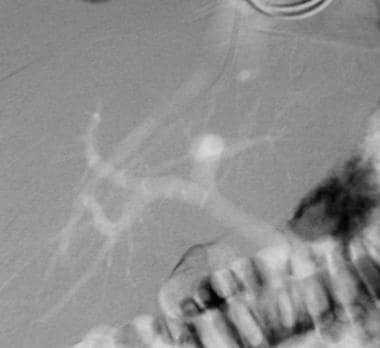
Basic transjugular intrahepatic portosystemic shunt (TIPS) procedure. A wedged hepatic venogram obtained by using the digital subtraction technique obtained with CO2 gas demonstrates the location of the portal vein. The catheter is wedged in a branch of the right hepatic vein.
View Media Gallery
Typically, a 50-mL manual injection of CO2 is used. This procedure usually reveals the location of the main PV, as well as the locations of left and right branches. Frequently, more than one CO2 injection is required to obtain a good portogram. If wedged injection fails to fill the PV, an occlusion balloon catheter may be used. Biplane CO2 wedged hepatic venograms and biplane fluoroscopy can be used.
With wedged hepatic venogram images used as a guide, the Colapinto needle is advanced through the wall of the right hepatic vein and is directed anteroinferiorly to access the right PV.
(See the image below.)

Basic transjugular intrahepatic portosystemic shunt (TIPS) procedure. Image demonstrates advancement of a Colapinto needle into the right portal vein.
View Media Gallery
Some have advocated injecting CO2 as the 21-gauge fine needle is advanced through the liver to more definitively guide the puncture. Once the portal vein has been cannulated, CO2 is injected into the parenchymal tract to exclude transgression of the bile duct or hepatic artery. If the bile duct has been transgressed, the access may be abandoned; if a small branch has been transgressed, a covered stent such as the Gore VIATORR TIPS Endoprosthesis is placed.
The Gore Viatorr polytetrafluoroethylene-covered stent (in 316 patients) was compared with standard uncovered stents (in 157 patients) for measurement of shunt function and clinical efficacy by Tripathi et al. Investigators found that the Viatorr covered stent had lower rates of shunt insufficiency (8% vs 54%), variceal bleeding (6% vs 11%), and hepatic encephalopathy (22% vs 32%). Mortality rates were similar for the 2 groups.
[24] Clark et al concluded that covered stents do not mitigate postshunt hepatic dysfunction and do not improve survival.
[25]
If a good wedged venogram cannot be obtained, an appropriate site for puncture from the hepatic vein to the PV is selected based on a thorough understanding of hepatic anatomy. The right hepatic vein lies superior and posterior to the PV bifurcation, and the right PV usually courses lateral to the T11 vertebral body. The portal bifurcation may be extrahepatic in a large percentage of patients. An extrahepatic puncture can lead to life-threatening hemorrhage, whereas puncture of a peripheral portal venous branch can create an angle that is too acute for successful TIPS placement.
From the right hepatic vein, the needle is usually aimed anteromedially and caudally, then is advanced 3-4 cm within the liver. Several punctures may be necessary for success. Large-volume paracentesis before TIPS in a patient with massive ascites can facilitate cannulation of the hepatic vein and puncture of the PV.
The needle is gently aspirated as it is withdrawn across the parenchymal tract. Once portal venous blood is freely aspirated, contrast material is injected through the needle to verify the point of entry into the vessel. An intrahepatic access site with entry into the right PV at least 1 cm from the main PV bifurcation is desired. A guidewire and a catheter are advanced into the PV, and portal venography is performed.
Pressure measurements are obtained in the PV as well as in the right atrium. The difference between measured pressures yields the portosystemic gradient. If the pressure gradient is significantly elevated (>12 mm Hg), the TIPS is placed. If the gradient is not elevated, the presence of a competitive shunt such as a spontaneous splenorenal shunt must be evaluated. Spontaneous shunts can be used to lower the portosystemic gradient, but they are not true vessels and lack normal vascular integrity, which poses a risk for rupture.
The intrahepatic parenchymal tract is dilated with an 8- or 10-mm high-pressure balloon such as the Conquest high-pressure balloon. Images of the initial balloon waist are saved because they show the locations of the PV entry site and the hepatic vein exit site. A self-expanding metallic stent such as the Wallstent is then deployed across the tract and is dilated to the desired diameter with use of an angioplastic balloon.
(See the image below.)
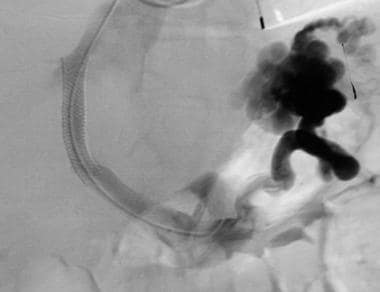
Basic transjugular intrahepatic portosystemic shunt (TIPS) procedure. A TIPS (10 X 68 mm Wallstent dilated with 10 mm X 4 cm balloon) has been placed. Note flow through the Wallstent and filling of the splenorenal shunt. The intrahepatic portal flow became reversed after TIPS placement.
View Media Gallery
Proper stent placement is crucial, especially if the patient is undergoing subsequent orthotopic liver transplantation. The stent should form a smooth and gentle curve and must extend adequately into the portal and hepatic veins. Overextension of a stent into the PV, the hepatic vein, or the inferior vena cava can be problematic for the transplant surgeon. The Wallstent significantly shortens as it is deployed, and ability of the surgeon to predict and achieve appropriate final stent placement improves with experience. Self-expanding nitinol stents that minimally shorten with deployment are available from multiple manufacturers, and one of these may be used to attain more predictable stent placement.
The stent may have to be dilated 8-12 mm, depending on the indication for TIPS and the stent used. Postplacement venography is performed, and pressures are measured to confirm adequate stent positioning, good flow through the TIPS, and reduction in the portosystemic gradient. If needed, additional stent placement or further balloon dilation can be performed to obtain a final portosystemic gradient of 8-12 mm Hg. Postplacement venography revealing persistent variceal filling indicates that insufficient decompression has been achieved with the stent. These varices can be selectively catheterized and embolized with coils.













![Toni Kroos là ai? [ sự thật về tiểu sử đầy đủ Toni Kroos ]](https://evbn.org/wp-content/uploads/New-Project-6635-1671934592.jpg)


