Fibromyalgia – A Difficult Diagnosis — The Holistic Health Approach
Fibromyalgia, a chronic pain condition, has become prevalent in the United States effecting an estimated 10 million Americans. As common as this condition is, healthcare practitioners still struggle with understanding its complexities. This means that if you suffer from fibromyalgia it could be a long road to diagnosis and treatment. But, knowledge is power. Understanding the symptoms, potential causes and treatment options may lead to a quicker diagnosis and getting your life back.
Symptomology
Fibromyalgia effects several systems in the body. The most common symptom is widespread chronic soft tissue pain that may be accentuated at certain tender points. However, this condition is commonly expressed with many other accompanying symptoms. In addition to pain, patients may suffer from:
-
Chronic fatigue
-
Disturbed sleep and unrefreshing sleep
-
Muscular stiffness and/or muscle twitching
-
Restless leg syndrome
-
Numbness, tingling and feeling cold in the hands and feet
-
Raynaud’s Phenomenon
-
Mood disturbances such as depression and anxiety
-
Cognitive difficulties
-
Balance problems and impaired coordination
-
Migraine and tension headaches
-
Temporomandibular disorder
-
Dry eyes and mouth
-
Sensitivity to bright lights or loud noises
-
Skin sensitivities
-
Chest pain and palpitations
-
Shortness of breath
-
Irritable bowel syndrome, diarrhea, constipation, bloating and cramping
-
Chemical and/or food allergies
-
Pelvic and urinary problems and/or interstitial cystitis
-
Painful periods and PMS
-
Sexual dysfunction
-
Weight fluctuations
In most cases, symptoms gradually present and slowly increase in intensity. As these myriad of symptoms and their severity continue to increase it can shatter the life of anyone suffering from fibromyalgia. But, what is even more devastating is the long road to diagnosis.
Diagnosing Fibromyalgia
Assessing a diagnosis of fibromyalgia is based on the Classification of Fibromyalgia criteria by the American College of Rheumatology (ACR). The criterion involves:
-
Widespread pain that has been present for at least three months.
-
Pain is bilateral as well as above and below the waist.
-
Pain is felt in at least 11 of 18 specific tender point sites, on both sides of the body.
The ACR has proposed additional diagnostic criteria to include common symptoms such as fatigue, sleep disturbances and cognitive problems as well as pain with a symptom severity score. However, the problem is not necessarily the diagnostic procedure.
One issue lies in the healthcare provider’s consideration of the disease. Some practitioner’s still believe fibromyalgia is just in the sufferer’s head. Other, well-intentioned practitioners consider other diseases first. There are no laboratory or imaging tests to diagnose fibromyalgia. Additionally, there is no tissue inflammation in the areas that present with pain. So the numerous symptoms that can present in each patient become distractions for the practitioner. Diagnosis only comes after a long process of eliminating other possibilities. This is not at the fault of the practitioner. Another issue with diagnosis is the etiology, or cause, of fibromyalgia – unknown.
Etiology
Although the etiology of fibromyalgia remains unknown, research has helped identify possible causes and underlying pathologies that may explain the symptoms and progression of the condition.
Dysregulation of the Autonomic and Neuro-Endocrine Systems. Studies have indicated fibromyalgia patients have unusually low levels of serotonin, ATP and growth hormone; elevated evening cortisol and high levels of Substance P. Low serotonin levels may contribute to pain sensitivity, sleep disturbances and mood disorders. Low ATP contributes to lack of energy and debilitating fatigue. Deficiency in growth hormone has been linked to increased pain severity and high levels of pro-inflammatory cytokines. Additionally, elevated evening cortisol contributes to sleep disturbances and nonrestorative sleep which, in turn may cause fibromyalgia related pain.
Of particular significance, however, is Substance P – a neurotransmitter that increases sensitivity to and awareness of pain. These neurochemical alterations may interrupt the central nervous system’s ability to process painful stimuli which can actually amplify pain perception.
Disturbed Stress Adaptation Response. The hypothalamic-pituitary-adrenal axis (HPA) is a critical component of the stress adaptation response. Excessive stress can cause alterations in corticotropin-releasing hormone and lead to an imbalance in the HPA axis. Dysfunction in the HPA axis has been demonstrated in fibromyalgia patients. Additionally, fibromyalgia can be triggered by stressful conditions, both mental and physical – overexertion, anxiety, lack of sleep, grief, trauma, extreme temperature and/or humidity, infections and illness.
Infections and Illnesses. Fibromyalgia may be triggered by some illnesses. According to research, there is a higher incidence of antibodies against enteroviruses in patients who have acute onset of fibromyalgia. It has been proposed that the Epstein-Barr virus, mononucleosis virus, Candida albicans fungus, chronic mercury poisoning from dental fillings, parasites, hypothyroidism, hypoglycemia and anemia may cause fibromyalgia related symptoms.
Inflammation. Although there is no sign of inflammation directly in the painful tissue, some evidence suggests an inflammatory process may be contributing to the onset and/or progression of the condition. Fibromyalgia frequently occurs with other chronic inflammatory conditions, such as arthritis and lupus, and patients commonly have high levels of pro-inflammatory substances like cytokines and substance P.
Genetics. It is common for fibromyalgia to run in families. Researchers have found several genes that may relate to your risk of developing fibromyalgia.
As you can see, the potential causes of fibromyalgia also have their own symptoms and underlying issues, making it difficult to pinpoint one specific cause for your symptoms. Additionally, the list of risk factors your doctor will know is limited and vague – being female, a family history of fibromyalgia and having osteoarthritis, rheumatoid arthritis or lupus. So, for example, if you are a male with rheumatoid arthritis and no family member already receiving a correct fibromyalgia diagnosis, your treatment will mostly likely end with the rheumatoid arthritis diagnosis. Another reason diagnosis is difficult is the unpredictable course and progression of the condition. Some cases clear up on their own, some become chronic and some are cyclical with intermittent remission between flare-ups.
Despite the difficulties, your healthcare practitioners can get the upper hand when they understand the possible causes, co-morbid conditions and numerous symptoms that can present. If all of these are considered during a differential diagnosis, a fibromyalgia assessment may come sooner allowing faster treatment and management.
Treatment
Conventional treatment of fibromyalgia includes both medications and nonpharmacologic therapy. Most experts agree that a multidisciplinary approach focused on treatment of pain, fatigue and sleep quality as well as improving emotional balance and physical capacity is effective.
Pharmacologic therapy includes pain relievers – both opioid and nonopioid, sleep aids, anti-inflammatories, antidepressants, muscle relaxants, anticonvulsants and even Botox injections in painful sites. Additionally, the FDA has approved 3 drugs for the treatment of fibromyalga – the anticonvulsant Pregabalin (Lyrica), the antidepressant Duloxetine (Cymbalta), and another antidepressant Milnacipran (Savella). One problem with pharmacology is that they are not effective for the entire scope of symptoms and many patients fail to respond to the medication. Another issue is the tendency of patients to be very sensitive to medications which increases side effects and their severity. In fact, narcotics should be used sparingly and steroids should be avoided if there is no concomitant rheumatic illness. Finally, patients often present with different symptoms and varied severities so there is no universal drug protocol to apply.
Nonpharmacologic therapies may be more effective than medications. Cognitive Behavior Therapy (CBT), biofeedback and relaxation techniques to reduce stress have been shown to reduce pain and improve sleep. Eliminating tobacco use and reducing excessive alcohol consumption have been strongly associated with decreased pain and fatigue. Some data suggests acupuncture can provide short term pain relief by triggering the release of endorphins. Even educating patients on the diagnosis and treatment of fibromyalgia has been effective at reducing symptoms.
However, two lifestyle modifications – exercise and nutrition – may be the key for patients to improve symptoms, reduce flare-ups and get their life back. Several studies show exercise is more effective in alleviating symptoms of pain, depression and sleep disturbances than medications. Exercise does not have to be strenuous either – restorative yoga, tai chi, and walking for a short duration have proven effective. Additionally, one study found eliminating allergenic foods significantly reduced pain and improved other symptoms including headaches, fatigue, bloating, heartburn and breathing difficulties.
Nutrition and Supplementation
Eliminating allergenic foods is not the only way to utilize food and nutrients to reduce symptoms and even prevent the onset or flare-ups of fibromyalgia. Your diet should be rich in vegetables, fruits, allergy-free whole grains, raw nuts and seeds, organic soy, skinless poultry, deepwater fish and plenty of liquids from distilled or filtered water and herbal teas. Fibromyalgia sufferers should also avoid caffeine, alcohol and sugar – all of which promote fatigue, increase pain and disturb sleep. Green peppers, eggplant, tomatoes and white potatoes contain solanine, a substance that interferes with enzymes in muscles and may cause pain and discomfort. Limiting consumption of these vegetables may reduce pain.
A vegetarian diet has shown to be beneficial for decreasing pain. However, the most important parts of the diet are consuming foods high in antioxidants as well as eating four to five small meals daily for a steady supply of nutrients to assist with proper muscle function.
Targeted supplementation may also help relieve symptoms. Below are certain nutrients to consider if you suffer from fibromyalgia*:
-
5-HTP may improve fibromyalgia symptoms of pain, fatigue, depression, anxiety and insomnia.
-
Melatonin has been shown to improve sleep and fatigue related symptoms.
-
SAMe has been linked to improvements in morning stiffness, fatigue, quality of sleep and relief from depression.
-
CoQ10 has been found to be lacking in fibromyalgia patients and supplementation may relieve symptoms of fatigue.
-
Acetyl-L-Carnitine may also be deficient in fibromyalgia sufferers. Trials have shown this supplement may improve pain and cognitive symptoms.
-
Omega 3 Fatty Acids have been linked to significant improvements in pain severity, tender point counts, fatigue and depression.
-
Magnesium is commonly low in the general population and many fibromyalgia patients are deficient.
-
B vitamins are important cofactors in several metabolic activities. Supplementing with a sublingual B complex may reduce symptoms of fatigue.
-
Vitamins A, C, E and the mineral zinc all provide antioxidant protection to complement a whole foods, high vegetable diet.
Having a healthcare practitioner who is willing to work diligently to understand and identify the root cause of your suffering can turn a difficult diagnosis into an easy protocol of lifestyle modifications, dietary changes and targeted supplementation. Reducing your time to diagnosis and providing clear cut guidelines may be able to not only improve your symptoms but return you to a normal life.
*Consult with your doctor before starting any supplementation protocol.
RESOURCES:
Prescription for Nutritional Healing, Phyllis A. Balch, CNC
Disease Prevention and Treatment, 5th Ed
Living Well with Autoimmune Disease, Mary J. Shomon
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3394355/
http://www.mayoclinic.org/diseases-conditions/fibromyalgia/symptoms-causes/dxc-20317796
https://newsinhealth.nih.gov/issue/feb2016/feature2
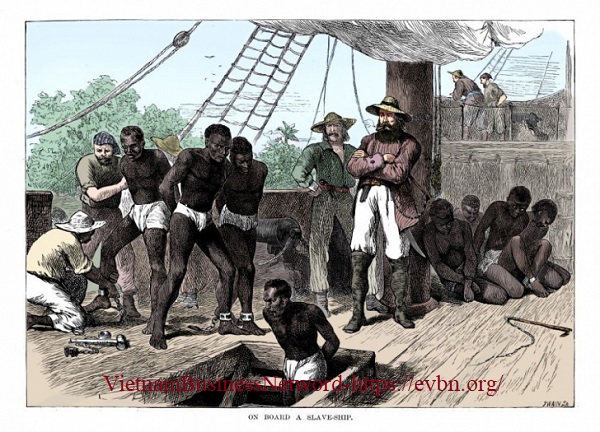
Photo Courtesy of:
http://briggschiro.com/fibromyalgia/













![Toni Kroos là ai? [ sự thật về tiểu sử đầy đủ Toni Kroos ]](https://evbn.org/wp-content/uploads/New-Project-6635-1671934592.jpg)


